Otitis media, a term that may sound unfamiliar to many, refers to a common condition that affects the middle ear. This inflammation can occur in people of all ages but is particularly prevalent in children.
It is a particularly painful infection causing swelling, pressure and blockage of the middle ear, that can lead to temporary loss of hearing and fever.

What causes Otitis Media?
Eustachian tubes are a pair of narrow tubes that connect each middle ear to the back of the throat, enabling them to regulate air pressure in the middle ear and drain normal secretions.
In children, the eustachian tubes are shorter, narrower, and more horizontal compared to adults. This anatomy makes it easier for bacteria and viruses from the upper respiratory tract to reach the middle ear, leading to infections.
When the eustachian tubes become infected, they swell and block mucus from draining, building pressure in the middle ear. This mucus is a breeding ground for bacteria, which then multiply and make pus that builds up in the middle ear, causing the infection and pressure.
Ear infections are not contagious, but upper respiratory tract infections, such as colds and flu, can lead to otitis media making them more prevalent in winter.
How can BLIS K12™ help prevent otitis media?
Otitis Media can be caused by both bacterial and viral infections.
BLIS K12™ is a live oral probiotic that has been proven to inhibit a range of bacteria that lead to Otitis Media. BLIS K12™ colonises and naturally competes with pathogens for the same binding site, effectively crowding out the bad bacteria.
On top of this BLIS K12™ naturally produces bacteriocins that actively target and destroy the cell wall of these pathogenic bacteria, helping prevent infection and maintain a healthy, balanced microbiome.
Common bacterial pathogens that cause otitis media are Streptococcus pneumoniae, Turicella otitidis, Alloiococcus otitidis, Streptococcus pyogenes and Moraxella catarrhalis – all of which have been shown to be inhibited by BLIS K12™.1
For viral infections, BLIS K12™ has been shown to stimulate Interferon Gamma and Secretory Immunoglobulin, both key antibodies leading to a much faster immune response and less severe infection.
What have clinical studies have shown?
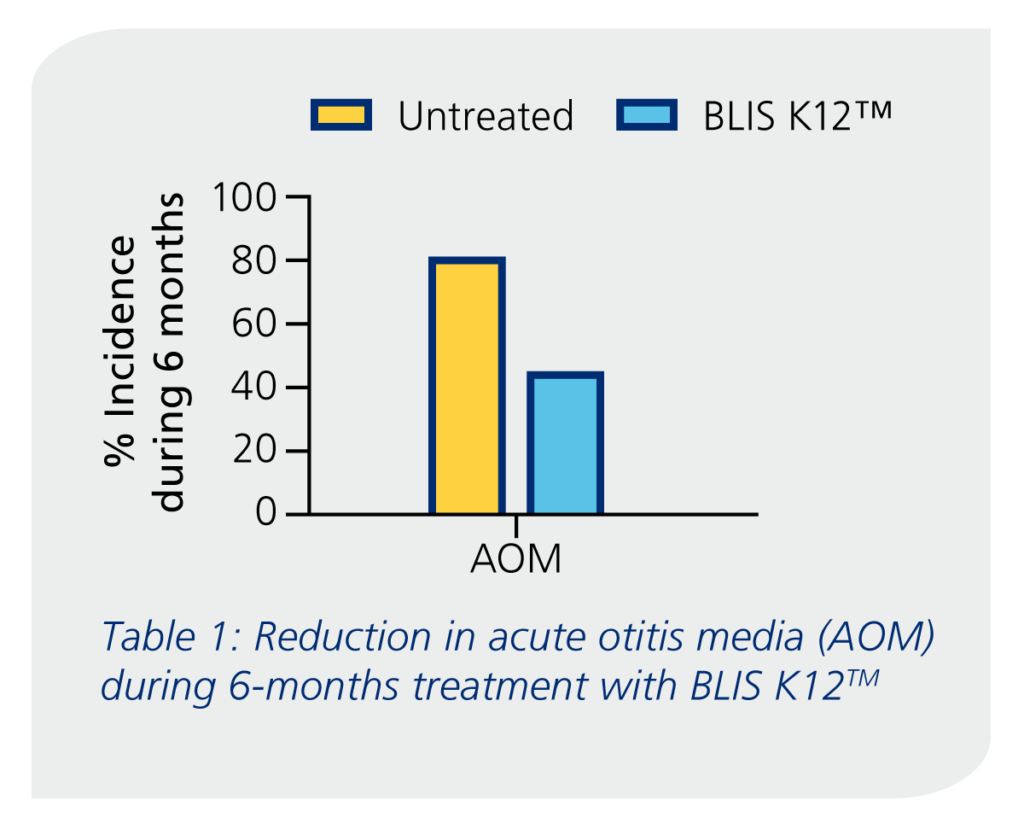
In a clinical trial completed by Di Pierro (2016)2 with 222 children aged 3 years old, showed the children who consumed BLIS K12 over a 6-month period had a reduced incidence rate of otitis media by 44.1% compared to 80.2% for the control group.
A second trial by Di Pierro (2018)3, with 133 children between the age of 3 and 14 years who were susceptible to otitis media had a reduced infection rate by 70% compared to the previous year.
In conclusion
Approximately 80% of children will experience otitis media during their lifetime, with many experiencing recurrent episodes. It is very painful and can lead to burst eardrums if not treated effectively.
BLIS K12™ is an advanced oral probiotic that helps prevent otitis media and a wide range of other upper respiratory tract infections by inhibiting the pathogens that cause infection.
Get in touch to learn more about BLIS K12™ and how it can be used as a key ingredient in immune health supplements:
References:
- Chen et al. In vitro Inhibition of Clinical Isolates of Otitis Media Pathogens by the Probiotic Streptococcus salivarius BLIS K12. Probiotics and Antimicrobial Proteins, 2021, 13(3), 734–738.
- Di Pierro, F., Colombo, M., Giuliani, M. G., Danza, M. L., Basile, I., Bollani, T., Conti, A. M., Zanvit, A., & Rottoli, A. S. (2016). Effect of administration of Streptococcus salivarius K12 on the occurrence of streptococcal pharyngo-tonsillitis, scarlet fever and acute otitis media in 3 years old children. European Review for Medical and Pharmacological Sciences, 20(21), 4601–4606.
- Di Pierro, F., Risso, P., Poggi, E., Timitilli, A., Bolloli, S., Bruno, M., Caneva, E., Campus, R., & Giannattasio, A. (2018). Use of Streptococcus salivarius K12 to reduce the incidence of pharyngo-tonsillitis and acute otitis media in children: A retrospective analysis in not-recurrent pediatric subjects. Minerva Pediatrica, 70(3), 240–245.